
Colon Cancer: A Silent Threat You Should Be Aware Of
According to 2022 statistics from the National Cancer Institute, Colon cancer is currently one of the top 3 most common cancers among the Thai population* It also contributes to increased mortality and reduced quality of life.
Colon cancer develops when abnormal cells in the colonic mucosa grow and form small polyps, which can then mutate into cancerous tumours. These tumours can spread to other parts of the body. Understanding the causes and risk factors associated with colon cancer, as well as undergoing regular screening, are crucial for prevention and reducing the risk of colon cancer
*According to 2022 statistics from the National Cancer Institute, colon cancer is the number 1 cancer in males and number 3 in females.
Table of content
What Causes Colon Cancer?
Medical specialists have identified three primary factors that contribute to the development of colon cancer: ” behaviour, genetics, and comorbid disease. “
Colon cancer is a complex disease influenced by a combination of genetic and environmental factors. Understanding these factors is the key to developing effective prevention strategies and reducing the risk of colon cancer.
Behaviours that Increase the Risk of Colon Cancer
Dietary Habits:
- Processed meats, such as sausage, ham, bacon, and hot dog, contain nitrates, which are known carcinogens.
- Diets high in fat and red meat, including grilled, barbecued, and fried meat, can produce carcinogens like polycyclic aromatic hydrocarbons (PAHs) and heterocyclic amines (HCAs).
A low-fibre diet can slow down bowel movements and increase the duration of exposure to carcinogens in the mucosa.
Alcohol Consumption and Smoking:
- Alcohol consumption can damage the colonic mucosa and increase the risk of colon cancer.
- Toxic substances in cigarettes, including nicotine and tar, can damage DNA, increasing the risk of colon cancer.

Physical Inactivity and Obesity
- A lack of regular physical activity can slow the digestive system and increase the risk of colon cancer.
- Being overweight or obese is a significant risk factor for many types of cancer, including colon cancer.
Inadequate Sleep
- In addition to the effects of diet and bowel movements, which can contribute to the risk of colon cancer, insufficient sleep is also linked to the disease (for example, having to wake up early for work or school and skipping breakfast). Research has shown that individuals who consistently sleep less than 6 hours per night have a 47% higher risk of colon cancer compared to those who get at least 7 hours.
Genetic Factors that May Contribute to the Risk of Colon Cancer
- Family History: Individuals with a family history of colon cancer, particularly among close relatives like parents or siblings,
- or with a family history of breast or ovarian cancer, can indicate an increased risk of colon cancer.
Diseases that May Contribute to the Risk of Colon Cancer
- Inflammatory Bowel Disease (IBD): For example, conditions like Ulcerative Colitis and Crohn’s Disease.
- Personal History of Cancer or Polyps: Individuals with a previous diagnosis of colon cancer or polyps have a significantly higher risk of recurrence.
How Colon Cancer Develops
Colon cancer typically begins with forming small, benign growths, called polyps, in the mucosa. If not detected and removed, these polyps can develop into cancerous tumours over time. This process can take several years and involves genetic changes within the mucous cells. These altered cells multiply uncontrollably and spread, eventually forming a malignant tumour.

Colon Cancer Symptoms
Early stages of colon cancer are often asymptomatic. Symptoms typically manifest in later stages (3-4); even then, they can be subtle and easily mistaken for other conditions. Awareness of potential warning signs is important, as early detection significantly improves treatment outcomes.
Changes in Bowel Movements:
Persistent constipation or diarrhoea, as well as noticeable changes in bowel movement frequency, either increased or decreased.
A frequent feeling of incomplete bowel movements, and pain or discomfort during bowel movements.
Stool Characteristics of Colon Cancer
- Stools may appear narrow (small), thin, or unusually long.
- Blood in the stool (either bright red or dark and tarry).
The presence of mucus in the stool.
Prolonged and persistent episodes of alternating hard and loose stools (or constipation and diarrhoea).
Abdominal Discomfort:
- Abdominal pain or cramping.
- Excessive gas, bloating, or feeling full quickly after eating.
General Symptoms:
- Unexplained and rapid weight loss.
- Unexplained fatigue or tiredness, which may be caused by anaemia.

Colon Cancer Screening and Prevention
Colon cancer screening is crucial for early detection and treatment. Screening can identify precancerous polyps. There are several screening methods available, comprising:
Colonoscopy:
This is a procedure in which a doctor uses an endoscope to examine the whole colon and rectum to detect cellular changes. If polyps are found, they can be removed for diagnosis and to prevent them from developing into cancerous tumours. It is generally recommended to start colonoscopy screenings at age 45-50, or earlier if you have a family history of colon cancer. It is recommended for those with no abnormalities to follow colonoscopy every 5-10 years. Colonoscopy is the standard method for colon cancer screening.
Imaging Tests:
For example, CT colonography, also known as a virtual colonoscopy, uses CT scan images to detect changes in the colon. This test is typically recommended every 5 years.
Flexible Sigmoidoscopy:
This procedure uses an endoscope to examine the sigmoid and rectum. It is often recommended every five years and may be combined with a faecal occult blood test.
Faecal Occult Blood Test (FOBT):
This test analyses a stool sample for hidden blood, which may not be visible to the naked eye. It should be performed annually, as detecting blood in the stool could indicate polyps or cancer.
Stool DNA Test:
This test detects DNA changes that indicate cancer or polyps. It is generally recommended every 3 years.
And these behaviours should be adjusted to help prevent colon cancer:
- Increase your intake of high-fibre diet.
- Limit your consumption of red meat and processed foods.
- Abstain from smoking and limit alcohol consumption.
- Engage in regular physical activity to maintain a healthy weight and promote a healthy digestive system.

Colon Cancer Treatment Options
Treatment options for colon cancer depend on several factors, including the stage of the cancer. Treatment options include:
Surgery
Surgery is the primary treatment for most cases of colon cancer. It involves removing a cancerous tumour and any affected part of the colon.
- Polypectomy and Local Excision: For early-stage cancer, surgery involves using an endoscope to remove a tumour from the colon.
- Partial Colectomy: This procedure involves removing the part of the colon that contains the tumour and then connecting the remaining sections of the colon together.
- Total Colectomy: This procedure involves removing the entire colon, which may be necessary in cases with multiple tumours or a high risk of cancer.
Radiation Therapy:
This procedure involves using radiation to destroy cancer cells, particularly in cases of rectal cancer, and may be used before or after surgery, or in conjunction with chemotherapy.

Chemotherapy:
This procedure involves using drugs to kill cancer cells or inhibit their growth. Chemotherapy can be administered before surgery to shrink the tumour or after surgery to reduce the risk of recurrence.
Immunotherapy:
This procedure involves using drugs to stimulate the body’s immune system to fight cancer cells. It is often used for colon cancer with specific genetic characteristics.
Targeted Therapy:
This procedure involves using drugs that specifically target and attack cancer cells while minimizing damage to healthy cells. Targeted therapy is frequently employed when cancer has spread to other organs.

The Seriousness of Colon Cancer (Colostomy Bag)
Colon cancer is considered one of the most frightening cancers due to its high death rate if not promptly and properly treated. Besides surgery and other treatments, some patients may require a colostomy bag to assist with bowel movements after colon surgery.
The Seriousness of Colon Cancer
- Metastasis: Colon cancer can metastasise to other organs, such as the liver, lungs, and bones, making treatment more challenging and complex.
- High Death Rate: If diagnosed at an advanced stage with metastasis, the chances of successful treatment decrease significantly.
- Impact on Quality of Life: Both colon cancer and its treatment may cause individuals to experience pain, discomfort, and alterations to their daily routines.
- Cancer Recurrence: While treatment is often successful, colon cancer can sometimes return, emphasizing the need for vigilant follow-up care and ongoing screening.
Colostomy Bag
The use of a colostomy bag in colon cancer patients involves surgically creating an opening in the abdomen to serve as a pathway for waste when the body’s internal pathways are unable to function normally. Colostomy bags are often necessary when a portion or all of the colon or rectum has been surgically removed.
Summary
Colon cancer is a significant and potentially deadly threat that requires vigilant attention. It carries a high death rate if not promptly and appropriately treated. Early-stage colon cancer is often asymptomatic. If there are abnormalities, it is usually an abnormality in bowel movements, typically noticed in later stages.
The primary factors contributing to the development of colon cancer are behaviour, genetics, and comorbid disease. Adjusting behaviours can reduce the risk of colon cancer, while regular screening enhances early detection and improves treatment outcomes. For individuals with no symptoms, screening is generally recommended starting at age 45-50, or earlier for those with a family history of colon cancer.
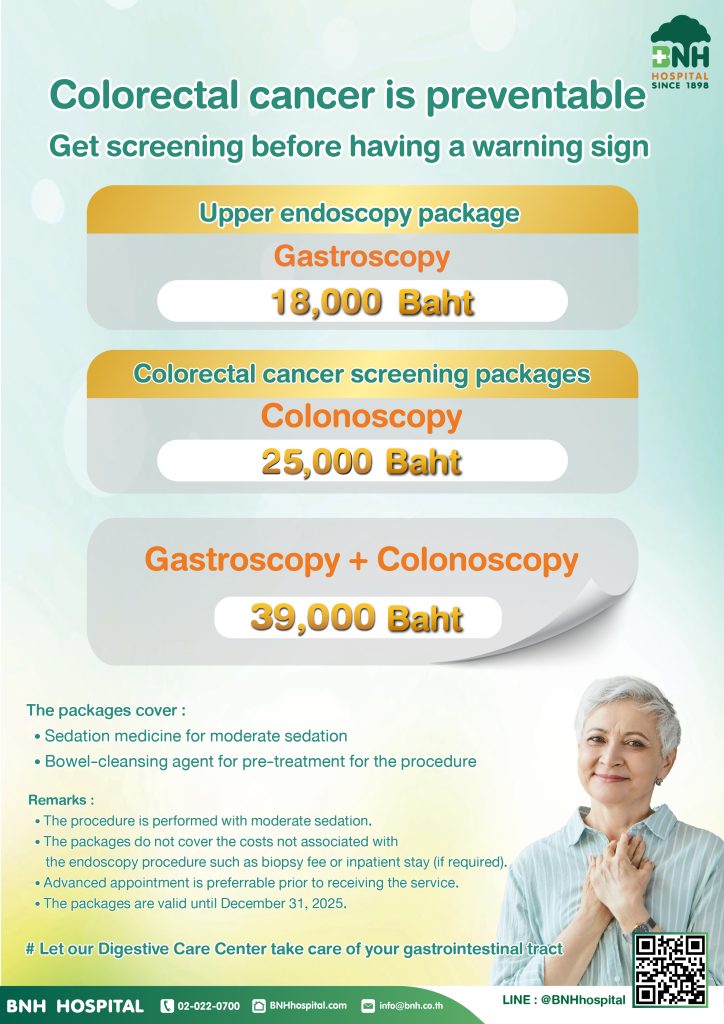
Gastroscopy & Colonoscopy Package
Another dangerous cancer that often appears without warning signs is colorectal cancer.
” Don’t be complacent! Colon cancer can be cured if detected at an early stage. “
Gastroscopy 18,000 THB
Include
- Doctor’s fee for gastroscopy
- Endoscopy room fee
- Preparation room fee
- Laxative medication fee
- Anesthesia fee (sedation)
- Medical equipment and instrument fee
- Hospital service fee
Colonoscopy 25,000THB
Include
- Doctor’s fee for colonoscopy
- Endoscopy room fee
- Bowel preparation room fee
- Laxative medication fee for bowel preparation
- Anesthesia fee (sedation)
- Medical equipment and instrument fee
- Hospital service fee
- Recovery room fee
Gastroscopy + Colonoscopy 39,000THB
- Doctor’s fee for gastroscopy
- Doctor’s fee for colonoscopy
- Endoscopy room fee
- Bowel preparation room fee
- Laxative medication fee for bowel preparation
- Anesthesia fee (sedation)
- Medical equipment and instrument fee
- Hospital service fee
- Recovery room fee
- Please make an appointment in advance.
- This price includes doctor fees and hospital service fees.
- This package includes an anaesthesia for the endoscopy (moderate sedation).
- This package does not include a general anaesthesia fee conducted by an anaesthesiologist, if required.
- This package does not include additional fees other than for the endoscopy itself, such as additional biopsy tests, room and board in the case of inpatient stay (admission), and medication and treatment of other illnesses.
Service Location: Digestive Care Centre, 3rd Floor, Zone B, BNH Hospital
Operating Hours: Monday–Sunday, 8:00 AM–5:00 PM.

Article By
SARANRAT TOEYWATANACHAI, MD.
Digestive Care Centre
Contact to inquire or make an appointment with staff via LINE @MBRACE.
Doctor’s Schedule
| Day | Time | Location |
|---|---|---|
| Monday | 08:00 – 19:00 | Digestive Care Centre |
| Tuesday | 08:00 – 17:00 | Digestive Care Centre |
| Wednesday | 10:00 – 18:00 | Digestive Care Centre |
| Friday | 08:00 – 16:00 | Digestive Care Centre |
| Sunday | 08:00 – 16:00 | Digestive Care Centre |







