- ×
 High Blood Sugar Package 1 × ฿2,790
High Blood Sugar Package 1 × ฿2,790 - ×
 BNH Luxury Postnatal Package Deposit 1 × ฿10,000
BNH Luxury Postnatal Package Deposit 1 × ฿10,000
4.4 Ladies-Go-Healthy | Pelvic Examination + Transvaginal Ultrasound + Bone Mineral Density Test 2 Parts: Lumbar Spine & Hip | BNH Hospital (Copy)
฿8,950
- Pelvic Examination
- Transvaginal Ultrasound
- Bone Mineral Density Test 2 Parts: Lumbar Spine & Hip
The package is available for purchase from April 1 – 15, 2024 via ONLINE channels only
(Services are valid until May 31, 2024).
Please show the purchase ‘Order Number’ to the staff on the day of using the service.
Out of stock


Love yourself, care your health from within
Get a regular women’s health check-up with our
4.4 Ladies Go Healthy package
Buy 1 Get 3 : Purchase one Ladies Go Healthy package and receive three health checks included.
The package is available for purchase from April 1 – 15, 2024 via ONLINE channels only
(Services are valid until May 31, 2024)
All women are susceptible to gynecological problems, which makes regular pelvic exams vital, irrespective of their sexual history. Early detection is key in finding common health risks and diseases and enabling timely treatment. It is important not to wait for symptoms to appear.
Who is this package suitable for?
Women of reproductive age and menopausal:
- Experiencing abnormal vaginal bleeding.
- Have a family history of gynecologic or colorectal cancer.
- Have a history of abnormal findings, such as ovarian cysts, chocolate cysts, or uterine fibroids.
- Women who want to have a regular pelvic exam.
Items included in the package
- Pelvic Examination is a physical examination performed by a gynecologist to check for abnormalities in the female pelvic organs, including the vagina, uterus, and ovaries, fallopian tubes and cervix.
- Transvaginal Ultrasound Transvaginal ultrasound (TVS) is an imaging procedure used to examine the pelvic organs, including the cervix, uterus, fallopian tubes and ovaries. It provides a more detailed view of pelvic organs than traditional abdominal ultrasound.
- Bone Mineral Density Test for lumbar spine & hip. A bone density test measures the bone mineral content and density for the diagnosis of osteoporosis.
Why is a pelvic exam important for women?
A pelvic exam is a physical examination performed by a gynecologist to check for abnormalities in the female reproductive organs, both internally and externally, which includes the vagina, uterus, ovaries, fallopian tubes and cervix. Some unexpected symptoms that women may experience and should be considered abnormal are
- Heavy menstrual bleeding
- Pelvic pain
- Painful periods
- Frequent urination
- Constipation or difficulty passing stool
See a gynecologist if you experience any of these symptoms, as they may indicate abnormalities.
Transvaginal ultrasound
Transvaginal ultrasound (TVS) is an imaging procedure that uses high-frequency sound waves to create images of female pelvic organs, including the cervix, uterus, fallopian tubes and ovaries. The ultrasound probe is inserted into the vagina to provide a clearer view of the pelvic organs compared to transabdominal ultrasound.
TVS is a valuable tool for diagnosing a variety of conditions, including:
- Uterine fibroids
- Ovarian cysts
- Endometriosis
- Pelvic inflammatory disease (PID)
- Uterine cancer
- Ovarian cancer
TVS is also used to monitor pregnancy and to guide procedures such as biopsies and IUD insertion.
Here are some of the benefits of TVS:
- It is a non-invasive procedure.
- It is relatively painless.
- It provides a clear view of the pelvic organs.
- It can be used to diagnose a variety of conditions.
If you are experiencing any symptoms that may be related to a pelvic organ abnormality, your doctor may recommend a TVS. This can help them to accurately diagnose the cause of your symptoms and recommend the appropriate treatment.

Preparation for Pelvic Exam and Transvaginal Ultrasound
- Having the exam at least 3 days after your menstrual period ends is recommended.
- Do not douche or use vaginal suppositories for 2 days before your exam.
- Avoid sexual intercourse for at least 1 day before your exam.
- If you are menstruating and have severe menstrual cramps, you can consult your doctor without waiting for your period to end.
- Wear comfortable, loose-fitting clothing, and empty your bladder before the exam.

Uterine fibroids
Fibroids are non-cancerous growths that develop in or around the uterus. They are also called leiomyoma or myomas. Fibroids vary in number and size. Many women have uterine fibroids sometime during their lives, but they might not know because of the absence of symptoms. Uterine fibroids are often found by chance during routine pelvic examination
Symptoms
- Many women who have uterine fibroids do not have any symptoms.
- Common symptoms of uterine fibroids include:
1. Heavy menstrual bleeding
2. Painful periods
3. Longer or more frequent periods.
4. Pelvic pressure or pelvic pain
5. Frequent urination
6. Growing belly
7. Constipation
8. Pain in the stomach or lower back, or pain during sex
Endometriosis
Endometriosis occurs when tissue similar to the lining of the uterus (the endometrium) grows outside the uterus.
Endometriosis affects up to 10 % of women of reproductive age. It often occurs on or around the reproductive organ in the pelvis or abdomen areas, including:
- Ovaries (Endometriotic cysts or Chocolate cysts)
- Fallopian tubes
- Ligaments around the uterus
- The lining of the pelvic cavity
- The outside surface of the uterus
- Space between the uterus and the rectum or bladder
More rarely, it can also grow on and around the bladder, cervix, intestines, rectum, abdomen, vagina or vulva.
The presence of endometrial tissue outside of the uterus can cause:
- Inflammation: This can lead to pain, particularly during menstruation.
- Scarring: This can lead to the formation of adhesions, which can distort the normal anatomy of the pelvis and cause pain and infertility.
Symptoms
The most common signs of endometriosis are pain and infertility.
Some women with endometriosis experience no noticeable symptoms at all.
The common symptoms of endometriosis include:
- Painful periods
- Pain during or after sex
- Pain with bowel movements or urination (before or during periods)
- Infertility
Ovarian Cyst
Ovarian cysts are fluid-filled sacs that develop on the ovaries. They are common in women of reproductive age, typically from 18 to 45.
Types of ovarian cysts:
- Functional cysts – These are the most common type of ovarian cyst. They form during the normal menstrual cycle and usually go away on their own.
- Endometriosis cysts – These cysts develop when tissue similar to the lining of the uterus (the endometrium) grows on the ovaries.
- Dermoid cysts – These cysts contain tissue from different parts of the body, such as hair, teeth, or skin.
- Cystadenomas – These are benign tumors that develop on the surface of the ovary.
Symptoms
Most ovarian cysts cause no symptoms, but a large ovarian cyst can cause:
- Pelvic pain: The pain can be sharp, dull, or achy, and it may come and go.
- Abdominal bloating
- Pressure or heaviness in abdomen

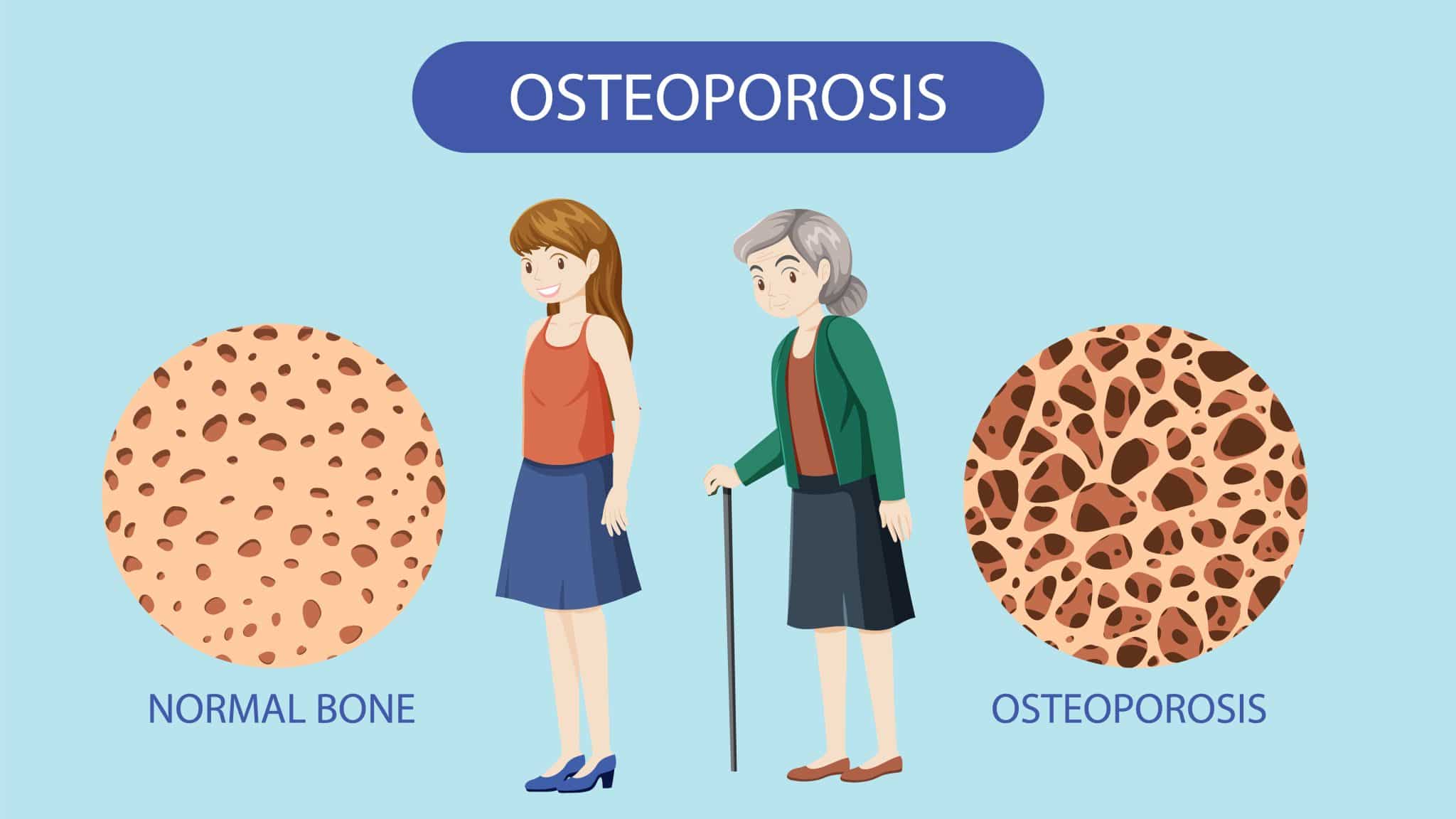
Osteoporosis in Women
Osteoporosis is a condition in which women lose bone mass and density, making their bones weaker and more likely to break. The most common sites of osteoporotic fractures are the wrist, spine, and hip. This condition is most common in women over 50, but it can occur at any age if bone health is not properly maintained.
Risk Factors for Osteoporosis
- Age – Bone mass peaks around age 30. After age 30, bone mass begins to decline slowly. The primary cause of bone loss is that new bone formation is slower than bone resorption. After age 50, bone loss occurs at an accelerated rate in both men and women.
- Gender – Women are more likely to develop osteoporosis than men due to two main reasons:
- Women have less bone mass than men. On average, women have 10-30% less bone mass than men.
- Women experience rapid bone loss after menopause. Estrogen plays a key role in maintaining bone mass. When women go through menopause, their bodies produce less estrogen, which leads to rapid bone loss.
- Genetics – It is true that children with parents who have osteoporosis are more likely to develop osteoporosis than the general population. However, this does not mean that children will always develop osteoporosis.
- Nutrition – Diet has a direct impact on osteoporosis. Inadequate nutrition affects bone mass formation and increases the risk of osteoporosis.
- Exercise – Lack of exercise directly affects osteoporosis. Low physical activity, infrequent exertion, and sedentary behaviour all increase the risk of osteoporosis.
- Body Shape and Balance – People with a body mass index (BMI) of less than 19 often have poor balance and mobility, which leads to frequent falls and increases the risk of osteoporosis more than people with normal body shape and balance.
- Chronic Diseases – Certain chronic diseases can lead to osteoporosis, such as endocrine disorders, inflammatory diseases, kidney disease, liver disease, malabsorption diseases, and cancer.
- Medicine – Certain medications, when used for long periods of time, can increase bone loss. Examples include steroids, thyroid replacement hormones, anticonvulsants, chemotherapy drugs, and psychiatric medications.
- Alcohol – It is important to avoid alcohol consumption, as it can accelerate osteoporosis and weaken muscles.
- Cigarettes – Nicotine in cigarettes affects bone mass formation, increasing the risk of osteoporosis.
How can osteoporosis be prevented?
- Eat a balanced diet – Eating a balanced diet provides your body with the nutrients it needs to build strong bones.
- Eat calcium-rich foods – Calcium-rich foods help build bone mass and prevent osteoporosis. Examples of calcium-rich foods include:- Dairy products such as milk, yogurt, and cheese
– Sardines and salmon
– Tofu
– Dried fish, shrimp powder, and fish powder
– Green leafy vegetables - Eat foods rich in vitamin D – Vitamin D helps your body absorb calcium better. Examples of foods high in vitamin D include:
– Dairy products fortified with vitamin D
– Egg yolks
– Fatty fish such as salmon, tuna, and sardines - Exercise regularly – Exercise helps strengthen bones, increase bone mass, and reduce the risk of fractures. You should exercise at least 3 days a week. Older adults should do weight-bearing exercises such as brisk walking, jogging, or dancing. They should also practice balance exercises to prevent falls.
- Make lifestyle changes – Avoid smoking, avoid excessive alcohol consumption, maintain a healthy weight. Preventing osteoporosis is important, especially for older adults. You should eat a healthy diet, exercise regularly, and make lifestyle changes to build strong bones and prevent osteoporosis.
How to Diagnose Osteoporosis?
There are several methods for diagnosing osteoporosis. The most common method used today is bone densitometry (BMD), which can measure bone strength and diagnose osteoporosis at an early stage. This method uses low-energy X-rays to reflect the image of bone tissue. The patient receives a low dose of radiation, and the results are quick, accurate, and safe.
There are several types of bone densitometers, but the most commonly used is the Dual Energy X-ray Absorptiometry (DEXA) scanner. The DEXA scan is used to measure bone density in the spine, hip, and wrist. These areas are the most common sites for bone fractures due to osteoporosis.
The DEXA scan is highly reliable and convenient, allowing for accurate assessment of bone strength.
Advantages of Bone Densitometry (BMD)
- To inform whether bones still have good density or if there’s osteoporosis
- Understand the risks and trends in disease occurrence. To prepare and prevent diseases related to bone strength that may occur in the future, such as fractures due to falls.
- Understand appropriate practices for treating bone strength. This includes precautions that should be taken specifically for each individual.
- Using test results as baseline data for comparing bone health in subsequent evaluations.
- DEXA Scan testing is easy, and quick, uses low levels of radiation that do not linger in the body, and provides accurate results.
Who Should Get a Bone Density Test?
- Women aged 65 years and older and men aged 70 years and older.
- Women who younger than 65 years old but have risk factors for low bone mass, such as low body weight (BMI less than 19 kg/m²) or a history of breast cancer.
- Men who younger than 70 years old but have risk factors for low bone mass, such as low body weight (BMI less than 19 kg/m²) or a history of prostate cancer.
- Individuals with a history of fragile bones and fractures, family history of osteoporosis.
- Individuals with diseases or conditions that affect bone mass, such as: Rheumatoid arthritis, Hyperparathyroidism, Diabetes, Chronic inflammatory diseases.
- Individuals who are taking certain medications that can reduce bone mass, such as: Steroids, Anticonvulsants, Cancer treatments.
- Patients who are about to start taking medication for osteoporosis
- Patients who need to be monitored for treatment response after receiving osteoporosis medication
- Individuals with risk factors, such as: Smoking or regular alcohol consumption, frequent consumption of tea, coffee, and carbonated drinks, lack of physical activity
Preparing for a bone density test.
- Remove all metal jewellery from your body.
- If you have any metal implants in your body, such as bone plates, artificial joints, or pacemakers, inform the staff before the test.
- Inform the staff if you are pregnant or suspect that you may be pregnant.
- If you have previously swallowed barium or received a contrast agent for a CT scan, consult your doctor to schedule the test at an appropriate time.
- During the test, you will lie on a bed. The staff will help you position your body properly before the test begins.
- The test takes approximately 10-15 minutes, depending on the number of areas to be examined.
For the good health of women, it is recommended to undergo regular health examinations to screen for risks of various diseases commonly found in women. Early detection allows the doctor to plan for prevention and treatment in a timely manner.
BNH Hospital Women’s Health Centre Tel. 02-022-0788, 02-0220850


 High Blood Sugar Package
High Blood Sugar Package  BNH Luxury Postnatal Package Deposit
BNH Luxury Postnatal Package Deposit 














